For decades, the foundations of cancer treatment have been surgery, chemotherapy, and radiation therapy. These methods, while crucial, often come with significant side effects and variable efficacy depending on the type and stage of cancer. However, the landscape of cancer treatment has been revolutionized by the advent of immunotherapies, particularly Chimeric Antigen Receptor T-cell (CAR T-cell) therapy.
What is CAR T-Cell Therapy?
CAR T-cell therapy is a form of immunotherapy that involves genetically modifying a patient’s own T cells to recognize and attack cancer cells. T cells, a type of white blood cell, are critical players in the body’s immune response. By engineering these cells to express chimeric antigen receptors (CARs), scientists have been able to redirect the immune system to target specific proteins found on the surface of cancer cells.
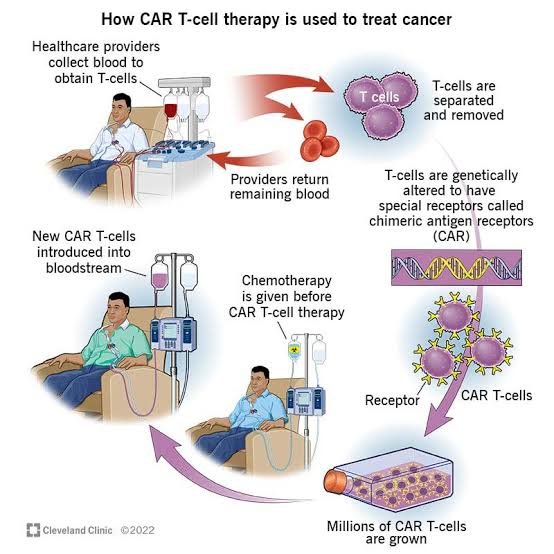
The process of CAR T-cell therapy involves several steps:
1. Collection: Blood is drawn from the patient, and T cells are separated from other blood components.
2. Genetic Engineering: A gene encoding the CAR is introduced into the T cells. This CAR is designed to bind to a specific antigen present on cancer cells.
3. Expansion: The modified T cells are then grown in large numbers in the laboratory.
4. Infusion: These engineered T cells are reintroduced into the patient’s bloodstream, where they seek out and destroy cancer cells.CAR T-cell therapy has shown remarkable success, particularly in treating hematological malignancies such as certain types of leukemia, lymphoma, and multiple myeloma. It has been approved by the FDA for these uses and has even led to complete remissions in some patients who had exhausted all other treatment options.
Recent Advances and News in CAR T-Cell Therapy
In recent months, CAR T-cell therapy has continued to make headlines due to its expanding applications and the development of next-generation CAR T therapies. Here are some of the notable advancements:
1. Solid Tumors: Historically, CAR T-cell therapy has been most effective against blood cancers. However, recent studies are exploring its application in solid tumors, which pose a greater challenge due to the complex tumor microenvironment and the presence of multiple antigens. Researchers are developing multi-targeted CARs and employing combination therapies to enhance the effectiveness of CAR T cells in solid tumors.
2. Enhanced Safety Profiles: The management of side effects, particularly Cytokine Release Syndrome (CRS) and immune effector cell–associated neurotoxicity syndrome (ICANS), has been a significant focus. The use of tocilizumab (Actemra), which targets the cytokine IL-6, has become a standard approach to managing severe CRS. Additionally, new strategies are being developed to mitigate neurotoxicity, a critical step toward making CAR T-cell therapy safer for a broader range of patients.
3. Universal CAR T Cells: One of the most exciting developments is the research into “off-the-shelf” CAR T cells, which are derived from healthy donors rather than the patient themselves. These allogeneic CAR T cells could potentially be produced on a large scale, reducing costs and making the therapy more accessible.
4. Longevity of Response: Recent long-term studies have provided insights into the durability of CAR T-cell responses. For many patients, the therapy has led to long-term remission, but there are still cases where the cancer returns. Understanding the mechanisms behind these relapses is a key area of ongoing research, with the goal of making CAR T-cell therapy a more permanent solution.
Challenges and Future Directions
Despite the successes, CAR T-cell therapy is not without challenges. The treatment is highly individualized, time-consuming, and costly. Moreover, while it has been life-changing for many, it is not universally effective. Some patients do not respond to the therapy, and others experience relapses. Researchers are working on next-generation CAR T cells with enhanced specificity and reduced side effects. There is also ongoing research into combining CAR T-cell therapy with other treatments, such as checkpoint inhibitors, to improve outcomes.
Conclusion
CAR T-cell therapy represents a significant leap forward in the treatment of cancer, offering new hope for patients with difficult-to-treat cancers. As research continues, the potential applications of this technology are expanding, bringing us closer to a future where cancer can be effectively managed or even cured with fewer side effects than traditional treatments. With ongoing advances, CAR T-cell therapy may soon become a standard part of the oncologist’s toolkit, transforming cancer care for millions of patients around the world.
Dr Sachin Jain,
DM (Oncology),
Cancer Specialist, Udaipur